That depends on who you ask. If you ask a medical doctor, gynecologist or endocrinologist, the answer will be yes or possibly a drug called spironolactone and Accutane for the acne. If you ask a naturopathic doctor, the answer will be “not by a long shot!”. There are numerous natural treatments for PCOS that can not only ease the symptoms, but also address the underlying cause of the condition and build up your body at the same time. Why the disparity in answers? Because Medical Doctors are not trained in and have little or no knowledge of naturopathic medicine. If you are looking for an alternative to drugs for PCOS, the best person to ask is not the person who is only trained in the drugs. It’s like asking your mechanic “what is the best dog food?” He or she may offer up an opinion on what to feed Rover, but it’s not coming from an expert on the subject. The best person to consult regarding natural remedies or alternatives to drugs for PCOS is a licensed naturopathic doctor who specializes in women’s health and PCOS.
Estrogen Metabolism or Clearing Excess Estrogen
Sex hormones are produced in the body via the following assembly line:
Cholesterol —-> Pregnenolone —-> Progesterone —–> Androstenedione —-> Testosterone —-> Estradiol (one form of estrogen). Estradiol is our end product and when there is the right amount of our end product, it’s the liver’s job to take any extra and break it down through a series of steps known as Phase I and Phase II liver detoxification. There are several ingredients required for successful breakdown and clearance of estrogen, as well as chemicals, pollution, pesticides etc. that can act like estrogen. We want to remove any excess estrogen and these waste products so that they don’t accumulate and do harm such as promoting reproductive cancers.
The first step in estrogen breakdown is conversion of estradiol to estrone. Estrone is then metabolised through Phase I liver detoxification (hydroxylation) into 2-hydroxyestrone. Cruciferous vegetables, flaxseeds, soy and rosemary supply substances like indole-3-carbinol that are necessary for this step to occur. The next step in estrogen breakdown is Phase II detoxification (methylation) which converts 2-hydroxyestrone to 2-methoxyestrone. This step requires vitamin B6, B12 and ACTIVE folic acid (5MTHF) to proceed. The active folic acid part is important as most folic acid from supplements is inactive. Some people have a defective gene that doesn’t allow them to process folic acid properly, so that they cannot make 5MTHF. This causes sluggish liver detoxification. There are 3 final procedures the liver can do to our 2-methoxyestrone to package it up for elimination. Glucuronidation requires glucaric acid, methlyation requires active folic acid again (5MTHF) and sulfation requires sulfur.
If any of these ingredients is missing, estrogen breakdown will be incomplete and estrogen, estrogen breakdown products and other waste like it, can build up in your system creating health problems like endometriosis, acne, fibroids, painful periods, hormone related cancers, heavy periods, infertility and other hormone imbalance conditions. In treating these conditions, I find it successful to provide (in the form of supplements) each component necessary for successful completion of phase I, phase II and the final packaging steps.
The typical benefits of enhancing estrogen metabolism this way include reduced risk of hormone related cancers, lighter periods, less cramping, less breast tenderness, reductions in fibroids, improved fertility, and clearer skin.
How Often Should I Do an Estrogen Detox?
That depends on the person and their particular symptoms, but for the average person, once per year.
Should Men do Estrogen Detoxification?
Yes! Men produce estrogen as well and excess estrogen and accumulation of estrogen like chemicals like bisphenol a, can bind to estrogen receptors in men and promote cancer such as prostate cancer.
Source: Medicine (Baltimore). 2015 Jan;94(1):e211 . Bisphenol a and hormone-associated cancers: current progress and perspectives. Gao H1, Yang BJ, Li N, Feng LM, Shi XY, Zhao WH, Liu SJ.
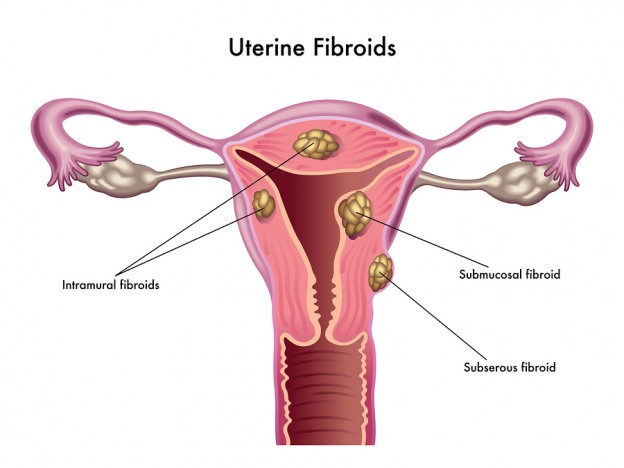
What’s New with Fibroids?
There’s a new drug on the market that is a “selective progesterone receptor modulator”. What that means is that the drug moderates the effects of progesterone. I have had a couple of patients on this medication prior to fibroid surgery and for both it does seem to have shrunk their fibroid. The thinking with fibroids has always been that estrogen was the culprit causing the fibroids to enlarge and in many of the women that I’ve treated for fibroids, that has been the case. However, in some fibroid patients, that’s not the case as demonstrated by the efficacy of this drug. For these women, we need more of a progesterone moderating approach.
How can we moderate the effects of progesterone naturally, without drugs?
- Ensure a healthy balance of all of the sex hormones so that no one hormone dominates over the others. That means two main things to me: a) keep insulin levels low by avoiding processed starches and sugars and b) keep the endocrine system working optimally, that includes the ovaries, thyroid, adrenal glands, pituitary and hypothalamus.
- Vitamin B6 in it’s active state, pyridoxal-5-phosphate (P5P) modulates the cell’s capacity to respond to steroid hormones. Although some of the professional lines contain the active P5P, most vitamin supplements don’t contain the active form of B6, relying on the body’s capacity to convert the inactive pyridoxine hydrochloride into the active P5P. Source: FASEB J. 1994 Mar 1;8(3):343-9.
- Scutellaria barbata is a Chinese herb that has been shown to have progesterone moderating and anti-proliferative effects. Source: Phytother Res. 2008 May;22(5):583-90
The 3 Worst Foods for Acne
There are three foods that I see causing problems with acne the most frequently:
- Dairy products – dairy is one of the most frequent food sensitivities there is. These are mild immune system reactions to foods that create inflammation. Acne is a very inflammatory condition, anything that provokes or increases inflammation in the body would be best to avoid. There is IgG Food Sensitivity testing that can be done to see if dairy is a food sensitivity for you, or you can try strictly avoiding dairy for at least 3 weeks to see what happens to your skin.
- Eggs – eggs fall under exactly the same category as dairy, they are a frequent food sensitivity and they create inflammation that seems to be centred in the skin. Eczema, psoriasis and acne can all be skin manifestations of an egg sensitivity.
- Sugar and processed carbs – high glycemic index starches and sugar provoke a high insulin response. Insulin in turn can increase the activity and/or the level of certain hormones, including testosterone. Higher testosterone activity or level can cause deep, painful cystic type acne.
The Benefits of a Detox for Women
Firstly, what exactly do I mean by a detox? Detoxification is the process whereby the liver breaks down toxins, chemicals, pollution, your own body waste and excess hormones. This process has to occur in order to make these garbage compounds into something the body recognizes as garbage so that they can be eliminated. If waste is not fully broken down, or detoxified, it can linger in your system and accumulate. The liver has two processes where it breaks these down called phase I and phase II liver detoxification. Certain vitamins, minerals and other substances from plants help ensure that this process runs smoothly, such as vitamin B6, vitamin B12, active folic acid (5 methyltetrahydrofolate or 5MTHF), indole-3-carbinol, glucarate, sulfur, N acetylcysteine and so on. If your body doesn’t have enough of these, toxins will get stuck in your system.
Because detoxification is part of the process to break down and excrete excess hormones, doing a detox can help:
- Acne
- Heavy periods
- Painful periods
- Infertility
- PMS symptoms
- Endometriosis
- Uterine polyps
- Fibroids
- Many other hormone related conditions.
Clearing toxins from your system can also reduce risk for hormone sensitive and other cancers.
Signs and Symptoms of Hormone Imbalance
How would you know if you had a hormone imbalance? Most of the women I see already have an inkling that something is out of balance by the symptoms that they are experiencing:
- Hair loss
- Acne
- Irregular periods
- Night sweats
- Hot flashes
- Infertility
- Heavy periods
- Painful periods
- Fibroids
- Ovarian cysts
- Uterine polyps
- Excessive facial or body hair
- PMS
- Premenstrual migraines
Most often they have already visited their family doctor who “checked their hormones” and told them “everything is normal” or offered them the birth control pill.
There are three main problems here:
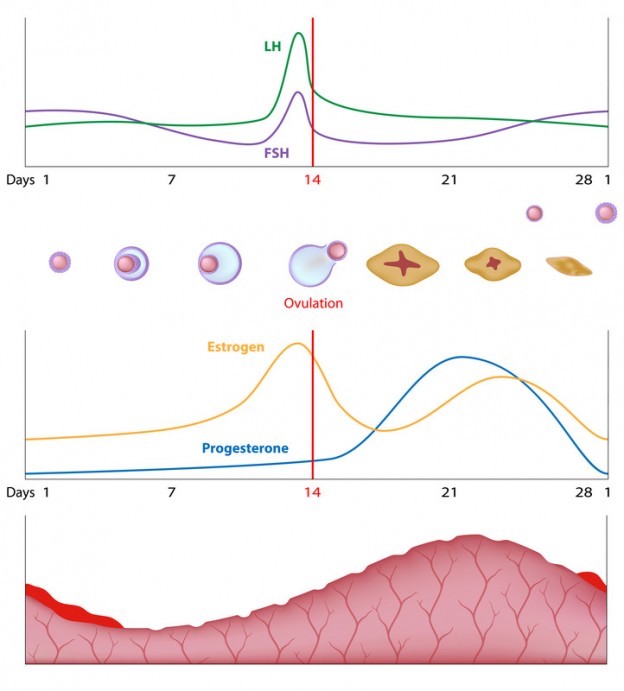
- By checked their hormones, most doctors mean they’ve done a very superficial screening of hormones, LH, FSH, maybe estradiol and maybe progesterone, but often not measured on specific dates of the menstrual cycle that make the results clinically meaningful.
- When “everything is normal” even though you feel that hormones are imbalanced, it’s because the “normal” ranges for hormones are extremely wide and so even abnormal people fall into the “normal” range.
- Birth control pills only mask the existing hormone imbalance, they don’t correct it.
If you feel like you have a hormone imbalance, always ask for a copy of blood work results so that you can see exactly how extensive testing was and exactly where your results fall in the “normal” range (normal is always in quotes because lab ranges rarely refer to what is actually normal, it is more often an average of unhealthy people). 99% of the time you will find that either: a) only a very few hormones have been tested and/or b) one or more of your results were borderline.
Is GSM Anything Like GMO?
Nope! GSM stands for Genitourinary Symptoms of Menopause. It’s a brand new diagnosis to encompass the symptoms women usually experience in the vagina and urinary tract with menopause. Menopausal and peri-menopausal women can tell you that there are some changes going on down there, and not exactly pleasant ones! The symptoms associated with GSM include overactive bladder, leakage, vaginal dryness and irritation, burning, pain or bleeding with intercourse, reduced arousal and libido, and recurrent bladder infections.
Having a new name for it doesn’t necessarily help you though. It’s the hormone changes associated with menopause that are responsible for these symptoms. While you can’t turn back the clock and reverse the hormones, there are herbs to keep hormones better balanced and nutrients like vitamin A, vitamin E and NAG among others that can help support healthy vaginal and urinary tract tissue.
Reference:
Portman D, Gass M. and consensus panel. Genitourinary syndrome of menopause: new terminology for vulvovaginal atrophy from the International Society for the Study of Women’s Sexual Health and The North American Menopause Society. 1063-1068
What Kind of Carbs Should I Eat?
The best kind of carbs are the ones that have minimal impact on blood sugar levels. High glycemic index and high glycemic load carbs (for example rice, wheat and wheat products) cause a sharp spike in blood sugar levels and insulin. A glycemic index of less than 55 is considered low and glycemic load of less than 10 is low. Rice, even if it’s brown rice, has a glycemic index of 58-84 and a glycemic load of 19-46. This will mean high insulin requirements to deal with the resulting spike in blood sugar.
So what’s wrong with that? Insulin’s job is to transport all of that sugar from the blood into the muscle, fat and other tissues and it causes the liver to store glucose as it’s storage form, glycogen. Once there is enough stored glycogen, the liver starts to produce fatty acids, which can be turned into triglycerides in fat cells, contributing to high blood lipids, atherosclerosis and fatty liver disease.
Insulin also preserves body fat, the more insulin the less breakdown of fat tissue. Not so good if you are trying to lose weight.
Insulin can also lower blood levels of potassium, a vital mineral for normal heart function.
Frequent insulin production, induced by frequent carb intake, can lead to insulin resistance or pre-diabetes. Insulin resistance can cause infertility, PCOS, heart disease, and is linked to an increased risk of cancer as both insulin and IGF1 have a role in tumor initiation and progression in insulin-resistant patients.1. How would you know if you were insulin resistant? Neither you nor your doctor would likely know until the point that your fasting blood sugar became abnormal, at which point you are diabetic. If you have PCOS you are already at a much higher risk of being insulin resistant and eventually becoming diabetic.
So what are the best kinds of carbs? Whole grain (not processed into bread, crackers, cereal, pasta), high fiber and lower glycemic index grains like quinoa, amaranth, lentils, beans and to a lesser extent spelt and kamut. Should you eat these at every meal? Probably not, best to give your body a break from the need to make insulin at every meal, even if it is a lower amount. Aim for small servings of lower glycemic index and load grains, once per day.
Have I Ever Put Anyone on a Zero Carb Diet?
No, because that is ridiculous. Unless you consumed nothing but water, you would have to be taking in carbs, even meat contains some amount of carbohydrate. For the average sedentary person, vegetables and fruit will supply sufficient carbohydrate for what your body needs. More active than usual? Great, add in a serving of one of the lower GI/GL carb sources listed above.
As a naturopathic doctor, it is my obligation to “do no harm”. If you suffer from a condition where frequent insulin production would do harm, like PCOS(2-6), I am bound by the Hippocratic oath to recommend decreasing carb intake and the need to make insulin. I’m happy to provide counselling and assistance in making the transition from a higher carbohydrate diet to a lower carbohydrate one.
1. Source: Exp Diabetes Res. 2012; 2012: 789174. Insulin Resistance and Cancer Risk: An Overview of the Pathogenetic Mechanisms, Biagio Arcidiacono, Stefania Iiritano, Aurora Nocera, Katiuscia Possidente, Maria T. Nevolo, Valeria Ventura, Daniela Foti, Eusebio Chiefari, and Antonio Brunetti.
2. Low carb ketogenic diet improves weight, percent free testosterone, LH/FSH ratio & fasting insulin in women with obesity & PCOS over a 24 week period. (Mavropoulos et al, Int J Endocrinol Metab. 2012)
3. PCOS patients ingesting a high protein diet experienced greater weight loss & body fat loss than the standard protein diet. (Sorenson et al, Am J Clin Nutr, 2012 )
4. In women with PCOS, consumption of a diet lower in CHO resulted in preferential loss of fat mass from metabolically harmful adipose depots, whereas a diet higher in CHO appeared to promote repartitioning of lean mass to fat mass. (Gossa et al, Metabolism, Oct 2014)
5. Energy restriction & weight loss in PCOS improve ovulation rates, conception, hyperandrogenemia, glucose & insulin levels, insulin resistance & satiety hormones. A low carb diet has an additional effect to caloric restriction in terms of weight loss. (Frary et al, Minerva Endocrinol, June 2014)
6. A diet containing 25% carbohydrates improved insulin resistance, whereas a diet that included 45% carbohydrates did not. Source: International Journal of Obesity and Related metabolic Disorders 20 no. 12:1067-1072
IBS and PCOS
What do these two things have in common besides being acronyms for common medical syndromes (Irritable Bowel Syndrome and Polycystic Ovarian Syndrome)? Recent research suggests that there is a connection between insulin resistance and leaky gut, which may then in turn cause irritable bowel syndrome. Want your gut to be healthier? Cut back on carbs and exercise daily to maintain normal insulin levels. Your hormones will be better balanced and you’ll be less prone to food sensitivities.
Menstrual and Premenstrual Migraines
For clues as to what may be causing premenstrual migraines, we have to look at what is happening hormonally at that time. On Day 21 of your cycle, progesterone is hitting a peak and estrogen levels are starting to rise a little to come to a second peak around day 23-24. By about day 25, assuming you are not pregnant or on the birth control pill, both levels are starting to fall which is the cue to your body to release the uterine lining and have a period. The peak of progesterone around day 21 is thought to be protective against migraines. The drop in estrogen is also thought to be associated with migraines. In the women that I have worked with who had premenstrual migraines, what has worked beautifully is an approach that optimizes progesterone production and balances estrogen.
1. Headache. 2008 Nov-Dec;48 Suppl 3:S124-30. doi: 10.1111/j.1526-4610.2008.01310.x. pidemiology and biology of menstrual migraine. Martin VT1, Lipton RB.
2. Headache. 2006 Mar;46(3):365-86. Ovarian hormones and migraine headache: understanding mechanisms and pathogenesis–part 2. Martin VT1, Behbehani M.